Jaundice- the yellowish discolouration of the skin that occurs in around 50% of full term well babies (and up to 80% of babies born prematurely). Most of us will have seen it at some point, but what is it, and what does it mean for your baby?

Newborn Jaundice
Jaundice is caused by a chemical called bilirubin. It is deposited in the skin and whites of the eyes, giving them a yellowish tinge. Bilirubin is released from red blood cells when they break down, or “haemolyse”. Red blood cells normally break down in the newborn period for a number of different reasons:
- Thick blood: Babies have a haemoglobin level of around 16-20g/dL compared to adult levels of 11-14g/dL, so it’s much thicker and more viscous. As the thick blood travels through the small blood vessels they are more likely to break down releasing bilirubin.
- Rapid rise in oxygen levels at birth: babies get used to low levels of oxygen in the womb; when they are born and start to breathe for themselves, the oxygen levels rise rapidly. This causes “oxidative stress”, leading to blood cell breakdown.
Sometimes, there can be other causes for increased red blood cell breakdown:
- Incompatibility between the mother’s blood type and the baby’s blood type: for example, if a baby is B+ and the Mother is O-, as fetal blood “leaks” across the placenta during pregnancy, the mother’s immune system detects the “foreign” B antigens and Rhesus antigens (the +). Mommy doesn’t have either of those antigens and assumes they need to be removed so her body develops antibodies to remove the antigens. These antibodies cross back over the placenta into the baby’s blood stream causing red blood cell breakdown and release of bilirubin.
- G6PD deficiency: G6PD is a chemical which makes red blood cells resistant to breakdown- without G6PD red blood cells are more prone to break- particularly within the first two weeks of life. G6PD deficiency is more common in people from Asian or Mediterranean races, and is seen more in boys than in girls.
Bilirubin may also also reach higher levels due to the newborn liver’s inability to convert the bilirubin into excretable forms, ready to be passed out of the body in the urine and stools. Breast milk itself possesses certain inhibitors which make jaundice last longer.
Finally, if breastfeeding is not going well, the baby may not pass sufficient urine and stool to remove the bilirubin from the body, causing it to build up.
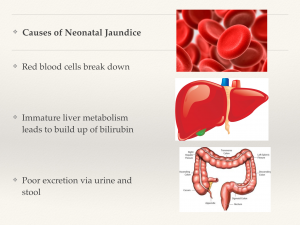
Causes of Neonatal Jaundice: Summary
Why Does It Matter?
Apart from making your baby’s skin and eyes yellow, why does it matter if your baby is a bit yellow?
Unfortunately , it’s not just about aesthetics. Bilirubin can cause permanent damage if not monitored and treated properly. Damage can range from impairment to the parts of the brain responsible for higher mathematic function, to permanent hearing loss, epilepsy, and even some forms of cerebral palsy.
Left unchecked, a baby with severe newborn jaundice may develop “kernicterus”: severe brain damage characterised by high-pitched screaming, poor feeding and back arching. This may lead to coma and, in the most serious cases, even death.
What Can You Do?
Fortunately, newborn jaundice is extremely treatable. Babies diagnosed and treated appropriately with blue light phototherapy have no long term damage at all. So, how do you make sure your baby is treated appropriately?
- Attend all scheduled routine doctor or health visitor check ups in the first two weeks following your baby’s birth: your doctor or health visitor will then be able to assess the baby and decide if a bilirubin test is required.
- Check if your baby is passing sufficient urine and stools: your baby should have at least one urine and stool output in the first day; this should increase to two to three on the second day and around four to five by day 3-4. By the end of the first week of life, your baby should be passing urine and stool around 6-8 times in a 24 hour period.
- Make sure your baby is not losing too much weight: it is usual for a baby to lose up to 10% of his birth weight in the first 3-5 days of life. He ought to be back to his birthweight by around day 7 to 10 of life, and be gaining around 200g per week thereafter.
Can I Suntan My Baby Instead Of Using Blue Light Therapy?
Blue light therapy has been the mainstay of treatment for newborn jaundice since the 1960s. It safely and effectively converts the bilirubin into an excretable form so that it can be removed from the body.
Sunlight does contain blue light, but also ultraviolet and infrared light, which may be harmful to babies. Some studies have recently used filtered sunlight (plastic panels that remove ultraviolet and infrared, but allow blue light wavelengths to pass through the filter) in resource poor settings in developing countries. These show significant promise. However, in developed countries, high levels of jaundice should be treated with appropriate blue light therapy.
Feel free to leave any comments below. And remember to subscribe by entering your email in the box above to receive medical and parenting information direct to your inbox. Have a great week ahead!
Leave A Reply